Clinical Case Study
Patient: Female, 14 years, 105 lbs Complaints Redness, pain and

Doug Richie, DPM, FACFAS, FAAPSM, Bruce Williams, DPM, and
James Clough, DPM, FACFAS, Neil Horsley, DPM, FACFAS
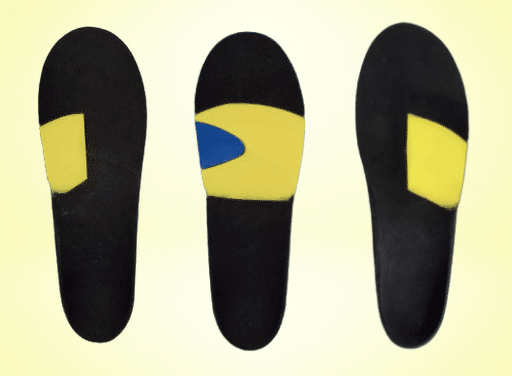
“Treatment of Morton’s neuroma is one of my most successful applications of foot orthotic therapy. Success can be achieved in all forms of footwear if the practitioner is creative in the prescription criteria,” says Dr. Richie. As he elaborates, the key to success is identifying and capturing a forefoot valgus deformity, which almost always accompanies this condition. Dr. Richie notes that balancing the forefoot valgus with intrinsic cast correction will reduce loading of the lateral column of the foot and offload the Morton’s neuroma.
For patients with Morton’s neuroma, Dr. Williams notes it is helpful to accommodate the area or use a metatarsal pad. In contrast, in Dr. Richie’s opinion, adding a metatarsal pad or “neuroma bump” is rarely helpful and often these pads cause too much pressure on the neuroma. Dr. Richie avoids rearfoot posting and tries to avoid full-length orthotics to allow preservation of the volume of the shoe. He also notes the importance of arch contour, especially for “dress orthotics,” in which simply supporting the arch can have very positive effects on relieving neuroma pain.
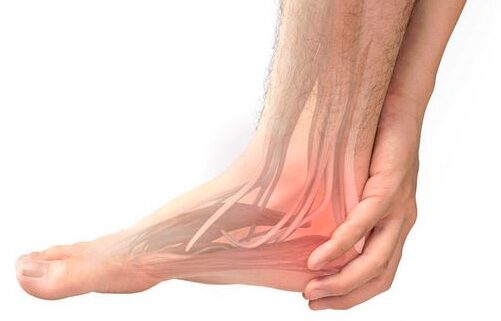
Dr. Williams says one will often need to add a 3 mm heel lift if the problematic foot suffers due to ankle joint equinus and/or a leg length discrepancy. As he explains, the heel lift will help equalize the forefoot and rearfoot pressures in a timely manner, and decrease the predominance of the forefoot pressures that occur in patents with neuromas.
Dr. Clough removes very few neuromas surgically, finding a neuroma is mainly a functional problem with lateral weightbearing on the forefoot in propulsion. This creates a strain on the fourth and fifth metatarsals, which he says actually have quite a bit of motion at the metatarsocuboid joint. Dr. Clough notes that this leads to a relative elevation of these rays and the development of a forefoot valgus. The second and third metatarsocuneiform joints are relatively locked in place and as a result, Dr. Clough notes there is a shearing between the mobile fourth metatarsal and the relatively immobile third metatarsal. He says the cause of this can be an uncompensated rearfoot varus, usually from a high degree of tibial varum.
However, Dr. Clough finds the most common cause of lateral forefoot overload is limited motion of the first MPJ. If patients cannot roll through the first MPJ, they will roll off the foot laterally to move forward. To correct this problem with plantarflexion of the first metatarsal, he suggests minimal orthotic fill. Additionally, Dr. Clough corrects any forefoot valgus by plantarflexing the fourth and fifth metatarsals, and adds minimal fill in the lateral arch just as he would do medially. For all such cases, he uses a P4 Wedge. “Very often, you also need to spend a few moments with your patients to get them to start to roll through the first MPJ and take a longer stride and walk faster without shuffling,” suggests Dr. Clough.
Dr. Horsley has found orthoses to be very effective for Morton’s neuroma. As he notes, when one designs orthotics with an accommodation to pocket the neuroma, it will dorsiflex the metatarsal heads directly adjacent to the neuroma. This will indirectly relieve the force from the deep transverse metatarsal ligament, according to Dr. Horsley. He notes the importance of accurately placing the accommodation for the neuroma.
However, Dr. Horsley notes varying degrees of neural involvement that will respond to appropriate conservative therapies. Low Dye strapping can provide improved function of the first ray and when there is an accompanying neuroma pad, he says this combination provides evidence that the orthoses will offer a similar level of pain relief along with improved function.
Are the symptoms directly related to the malfunction or instability of the first ray in combination with an equinus deformity? Is this condition referred pain from a tarsal tunnel syndrome? Dr. Horsley suggests a thorough physical evaluation and appropriate testing can assist in differentiation. If Morton’s neuroma is the final diagnosis, in this instance, he suggests control of the first ray, accommodation for the neuroma and intervention for the equinus with stretching and appropriate heel lifts.
Patient: Female, 14 years, 105 lbs Complaints Redness, pain and

We normally post articles about specific pathologies or cases of
The plantar fascia is a band of connective tissue running
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |